Melanoma is less common but more dangerous than other types of skin cancers. Melanomas are cancers of the pigment-producing cells in the skin, known as melanocytes. Normally these cells produce melanin which protect the skin from UV damage from the sun. When melanocytes become cancerous, they have the ability to grow rapidly and develop into malignant tumors, making melanoma a serious and life-threating disease. Melanomas can arise within an existing mole, but most develop on normal skin. Skin self-exams are encouraged and can help find concerning lesions when they are still very treatable. Early diagnosis and treatment is the best course of action.
Tues: 8:30am - 3:00pm
Wed: 12:00pm - 6:00pm
Thurs: 8:30am - 3:00pm
Fri: Closed
Sat: 8:30am - 12:30pm
Sun: Closed
Greenvale, NY 11548
Melanoma
What is melanoma?
What causes melanoma?
Like other forms of skin cancer, melanoma is most often triggered by regular exposure to ultraviolet (UV) radiation over time, either from natural sunlight or tanning beds. The UV rays impact the body’s DNA, which triggers the formation of tumors in the pigment-producing melanocytes in the basal (outermost) layer of your skin. Melanomas may resemble moles. Most are black or brown, but may also be skin-colored, pink, red, or even purple, blue or white. People with light skin, red or blond hair, freckles and other physical traits may be genetically at greater risk of developing melanoma. Studies have shown that the use of indoor tanning beds before the age of 35 increases the risk of melanoma by 59 percent, with the risk increasing with each visit to the tanning bed.
How dermatologists diagnose melanoma
Your dermatologist will examine the affected areas of your skin and ask questions about your medical and family history as well as your symptoms and when they first began. During the exam, your dermatologist will check the size, shape, color, and texture of the affected areas. Your dermatologist may use a dermoscopy instrument for close inspection of your skin. This device uses a magnifying lens and light source to view the area more clearly. Dermoscopy aids in making an accurate diagnosis.
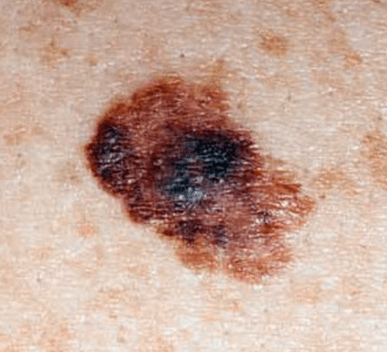
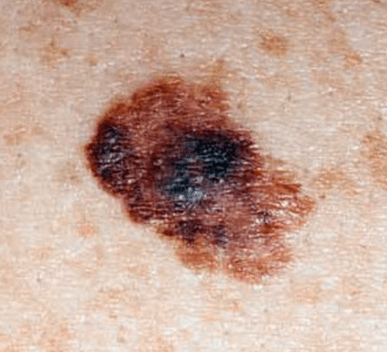
The following clinical features are warning signs to help detect melanoma, which are referred to as the ABCDEs of melanoma:
- A: Asymmetry – one half of the lesion does not look like the other half
- B: Border – there is an irregular or poorly defined border to the lesion
- C: Color – variation in color within the lesion including different shades of tan, brown, blue or black or sometimes even white or red
- D: Diameter – lesions greater than 6mm (larger than a pencil eraser)
- E: Evolving – lesions that are changing in size, shape, or color
A biopsy is necessary to confirm the diagnosis. A biopsy is an in-office procedure where your dermatologist will numb the skin around the affected area and remove the lesion for further microscopic evaluation.
If the lab report confirms melanoma, your dermatologist will have a detailed discussion about the stage of the melanoma. This information is important to help determine the prognosis and treatment options. There are five stages of melanoma skin cancer. Stage is based on tumor thickness, lymph node involvement and spread to distant sites.
Stage 0 (also known as In situ): Melanoma is confined to the top layer of skin.
Stage I: Melanoma is still confined to the skin but has grown thicker. In stage IA, the skin covering the melanoma is still intact. In stage IB, the skin has an open or ulcerated appearance under the microscope.
Stage II: The melanoma has increased in thickness, with or without breaking open on the surface.
Stage III: The cancer has spread to the lymph nodes or across the skin where the melanoma was first detected but has not spread to other parts of the body.
Stage IV: The melanoma has spread to internal organs or has developed on skin far from the original site of the development of the melanoma.
How dermatologists treat melanoma
Treatment of melanoma is individualized and based on the stage and personal medical history of each patient.
If a melanoma is diagnosed in the early stages, removal with surgery may be the only treatment required. With surgery, cure rate for stage 0 melanomas is close to 100 percent.
In advanced stages, when the melanoma has spread deeper or wider than the top layer of the skin, more aggressive treatment will likely be required. This may involve having the melanoma removed by a specialized surgeon or surgical oncologist (specialist in cancer surgeries).
A combination of other therapies may also be necessary to treat the cancer. These include:
- Lymphadenectomy, which is surgery to remove lymph nodes that have or may become affected by the melanoma.
- Radiation, which is a painless procedure that’s similar to getting an x-ray, only the radiation is stronger and focused directly on the cancerous area to kill the cancer cells. Radiation therapy can affect normal cells as well with side effect including hair loss, skin irritation and changes in skin tone.
- Chemotherapy, which involves taking medications orally or intravenously on a preplanned schedule. Chemotherapy is usually limited to advanced stages where the melanoma has spread into the lymph nodes and other body organs.






